What is Keratoconus?
Keratoconus is a bilateral (both eyes), non inflammatory condition characterized by steepening, thinning, and bulging of the cornea.
The cornea is the clear surface on the front of the eye and is critical for focusing light into the back of the eye where the light is captured and sent to the brain.
Instead of a smooth cornea, bulging from keratoconus causes a “cone” shaped cornea that distorts light as it enters the eye (above). In fact, in Greek Keratoconus literally means cornea, Kerato, that is cone shaped, Conus.
Who gets Keratoconus?
Keratoconus was once thought to be fairly rare (1:2000) but in reality is very, very common. Newer studies with better imaging technology revealed this condition affects about 1 in 375 individuals¹. This condition is present in all parts of the country and the world. There are no known gender, cultural, geographic, or socioeconomic risks factors.
Keratoconus usually develops in the mid to late teens and gets progressively worse through the 20’s and 30’s before stabilizing. However with milder cases, it is not uncommon for it to go undetected until much later on in life.
What Causes Keratoconus?
For the most part, this disease most often develops purely at random.
Family history and genetics are important but oddly a positive family history is only present in about 5 – 10% of cases².
Yet, one very interesting and well established risk factor for keratoconus is eye rubbing. Most noteworthy is the landmark Collaborative Longitudinal Evaluation of Keratoconus Study (CLEK Study) that showed 50% of patients surveyed admitted to rubbing their eyes frequently5.
While this connection is not completely understood, it is thought that repeated mechanical rubbing of the spongy, elastic cornea leads to break down of the corneal structure resulting in thinning and bulging. Consequently, patients with Keratotoconus and ocular allergies need treatment to decrease the eye rubbing which can lead to progression of this condition.
Furthermore, old contact lens fitting patterns suggested to “smoosh” down the bulging cone with a hard contact lens. However, the “rubbing” of the contact lens on the bulging cone will only cause further progression as well as additional mechanical damage and permanent scarring.
Is Keratoconus Blinding?
While this condition is quite common, it rarely cause blindness. Rather, specialty hard contact lenses often return vision to near normal levels and greatly improve quality of life.
 While specialty contact lenses are useful for Keratoconus, surgical intervention is sometimes needed due to the severity and/or rapid rate of progression. Historically, about 12 – 20% of patients developed complications that required a corneal transplant³. This surgery is known as a Penetrating Keratoplasty or PKP (right) and uses donor tissue to replace the thinned and scarred part of the cornea.
While specialty contact lenses are useful for Keratoconus, surgical intervention is sometimes needed due to the severity and/or rapid rate of progression. Historically, about 12 – 20% of patients developed complications that required a corneal transplant³. This surgery is known as a Penetrating Keratoplasty or PKP (right) and uses donor tissue to replace the thinned and scarred part of the cornea.
Another newer procedure recently (FINALLY!!) approved by FDA is called Corneal Cross Linking or CXL. Corneal Cross Linking uses riboflavin (vitamin B2) and ultraviolet light to greatly strengthen and stabilize the collagen network of the cornea.
The conclusion in numerous studies here and abroad show CXL successfully halts the progression and severe complications of Keratoconus by at least 93%4!!
Corneal Cross Linking has been a mainstay of treatment around the world for well over a decade. As a result of the recent FDA approval and the recent surge in CXL studies and limelight here in the US, this procedure will become more and more common place in the very near future.
With earlier detection and prompt treatment with CXL, the need for Penetrating Keratoplasty will likely (and thankfully) decrease dramatically in the years to come.
Read more about surgeries for Keratoconus and other corneal ectasia here.
How is Keratoconus Diagnosed?
 The symptoms of Keratoconus are usually quite nonspecific, such as blurry vision, glare, and halos around light. Often time patients simply present for an exam thinking they need stronger glasses or contact lenses.
The symptoms of Keratoconus are usually quite nonspecific, such as blurry vision, glare, and halos around light. Often time patients simply present for an exam thinking they need stronger glasses or contact lenses.
In addition to a complete ocular health exam, special testing with Corneal Topography is the best way to diagnosis Keratoconus.
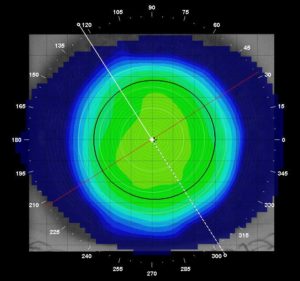
Topography is a very simply, painless procedure where an instrument maps out the curvature of the cornea. This data is similar to a geographical topographic map that shows hills and valleys. Above is a topography of a normal cornea, note the symmetrical, smooth contour of the surface.
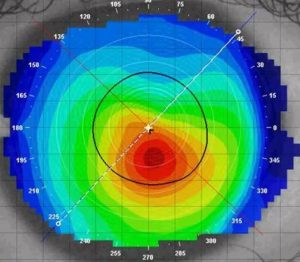 Compare that with an eye with keratoconus (left). This topography clearly illustrates the large bulging cone and the irregular surface.
Compare that with an eye with keratoconus (left). This topography clearly illustrates the large bulging cone and the irregular surface.
In addition to diagnosing Keratoconus, topography also shows the type and severity of the disease and lets the specialty contact lens fitter decide what contact lens would best help maximize vision.
Here is additional medical information for staging the type and severity of Keratoconus.
What Options do I have to See Better?
 The reason that Keratoconus causes blurry vision is because of the irregular corneal surface distorting incoming light. Therefore, any solution must counteract or mask the irregular corneal surface. Glasses will only help to mild degree because light still needs to travel through the irregular cornea, after the glasses. Similarly, soft contact lenses will just drape across the irregular surface and not greatly improve vision.
The reason that Keratoconus causes blurry vision is because of the irregular corneal surface distorting incoming light. Therefore, any solution must counteract or mask the irregular corneal surface. Glasses will only help to mild degree because light still needs to travel through the irregular cornea, after the glasses. Similarly, soft contact lenses will just drape across the irregular surface and not greatly improve vision.
As a result, mainstay of correction for decades has been some form of hard contact lenses. Specialty hard lenses hold their shape as they sit on the front surface and cover over the irregular cornea. At the same time, the tears fill in the space between the lens and the bulging cornea forming a new smooth front surface. In essence, this creates a new, prosthetic cornea resulting in vastly improved quality of vision.
Hard lenses designed for Keratoconus come in 3 main types:
Links Below to their dedicated pages with more info.
Specialty, small diameter hard lenses
Hybrid lenses: hard contact lens center and soft contact lens skirt
Scleral Contact Lenses: very large diameter hard lenses that rest on the white of the eye
There is no cure, but Keratoconus IS manageable.
In conclusion, all options have their benefits and draw backs and some are better for certain types and stages of Keratoconus than others. We will work with you to find a solution that best fits your needs.
If you have been struggling with the vision and/or comfort of your specialty contact lenses, please call us.
If you or a loved one has been recently diagnosed with this condition and you have questions, please call us.
At Precision Family Eye Care, we are confident in our ability to improve your vision and change your quality of life.
Excellent Additional Resources:
References:
- Godefrooji DA, de Wit GA, Uiterwall CS, et al. Age-Specific incidence and prevalencer of keratoconus: a nationwide registration study. AM J Ophthalmol. 2017 March; 175:169-172
- Gokhale, NS. Epidemiology of Keratoconus. Indian J Ophthalmol. 2013 August; 61(8): 382-383
- Shalchi Z, Wang X, Nanavaty MAA. Safety and Efficacy of epthelium removal and transepithelial cornea collagen crosslinking for keratoconus. Eye (long). 2015;29(1):15-29
- Wagner H, Barr JT, Zadnik K. Collaborative Longitidinal Evaluation of Keratconus (CLEK). Cont Lens Anterior Eye, 2007 Sep;30(4):223-32



