Contact Lens wearers of the world, meet one of the greatest enemies of successful contact lens wear:
Giant Papillary Conjunctivitis or GPC.
“My contact lenses wear out REALLY fast, I am constantly changing them!”
“I just can’t wear the contacts very long, they’re always moving on my eye.”
“I’m getting this weird stringy, white goop when I wear my contacts.”
What is Giant Papillary Conjunctivitis?
 Giant Papillary Conjunctivitis, or GPC as it is commonly known, is an inflammatory condition involving the conjunctiva of the human eye.
Giant Papillary Conjunctivitis, or GPC as it is commonly known, is an inflammatory condition involving the conjunctiva of the human eye.
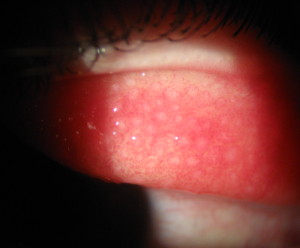
The conjunctiva is the thin slippy tissue that covers the front of the eyes as well as the inside of the eyelid. The hallmark of this condition are small (and sometimes GIANT!) bumps called papillae that form on the underside of the upper eyelid.
This is very chronic condition and can range from mild, to moderate (such as our patient pictured left), to very, VERY severe (If you are squeamish, DO NOT CLICK!).
Holy Crap! What Causes These Bumps?
At its core, GPC is an allergic condition and occurs almost exclusively in contact lens wearers (90 plus percent). It can also rear its ugly head with patients (like myself) who have very severe allergies – and in the Ohio River Valley, there are lots of us!
“It is estimated that up to 35% of extended wear contact lens wearers with develop symptomatic Giant Papillary Conjunctivitis.”
With contact lens wearers every individual is different. These bumps frequently form with certain types or brands of contact lenses, from the chemicals in contact lens cleaning solutions, or from overwear/abuse of contact lenses.
This is essentially a mechanical problem.
The brain is physiologically wired to blink the eyes every 10-12 seconds. Every time a blink occurs the underside of the lid rubs against the contact lens. Deposits, chemicals, and/or allergens on the contact lenses will begin to irritate the conjunctiva of the upper eyelid. With each blink these inflamed papillae begin to form, multiply, and expand making the symptoms worse and worse.
Why do these “bumps” cause me problems?
 Think of these papillae bumps like the grit on sandpaper.
Think of these papillae bumps like the grit on sandpaper.
- With each blink, these ‘sandpapery’ bumps rub, push and pull the lens around making it uncomfortable to wear.
- The bumps also poorly wet the lens making deposits form quicker. This results in the need to change your contacts far more frequently.
- Finally, the areas between the bumps allow mucus to form leading to an irritating, stringy, and often blurring mucus that coats the eye.
Not to mention that as the papillae bumps multiply and grow, the rubbing on the contact lenses increases making the symptoms worse and the bumps bigger – a death spiral for contact lens wear.
What do we do about it!
 Well, the problem here is that when the papillae are mild, the symptoms usually get shrugged off or put up with for months or even years.
Well, the problem here is that when the papillae are mild, the symptoms usually get shrugged off or put up with for months or even years.
Once the symptoms are bad enough that the contact wearer come in because the contacts “aren’t working”, the Giant Papillary Conjunctivitis is usually quite ‘ground in,’ severe and chronic.
If this condition IS caught early, a simple change to Daily Disposable lenses is usually sufficient. Daily Disposable lenses are replaced every day which means there is no time for deposits or allergens to attach to the lenses. Additionally, there is no solutions needed for Daily Disposable lenses which removes a lot of cleaners and chemicals that contribute to the papillae bumps.
For severe problems unfortunately, there is NO simple solution and the treatment usually consists of several steps.
- First step is discontinuing ALL contact lens wear. It doesn’t matter what lens we put on your eye at this point, it’s going to get manhandled by those BIG bumps!
- Since this is an inherent inflammatory reaction, we will start you on steroid eye drops for a period of weeks to months. Since this is a chronic condition, it often takes a long time to reduce these bumps to a level acceptable for comfortable contact lens wear.
- Once the Giant Papillary Conjunctivitis is under control, we will fit you will Daily Disposable lenses to keep this from happening again.
Other treatment options for this condition included discontinuing contact lenses all together or exploring the possibility of a surgical solution to refractive error through LASIK surgery.
If you are a contact lens wearer and have noticed these symptoms in your eyes. Please consider scheduling an evaluation with your eye care provided. With Giant Papillary Conjunctivitis, an ounce of prevention is worth a pound of cure.
If you have any questions about this topic or any others, please contact me at [email protected]
Take care of those eyeballs!
- Nick Wolf, OD



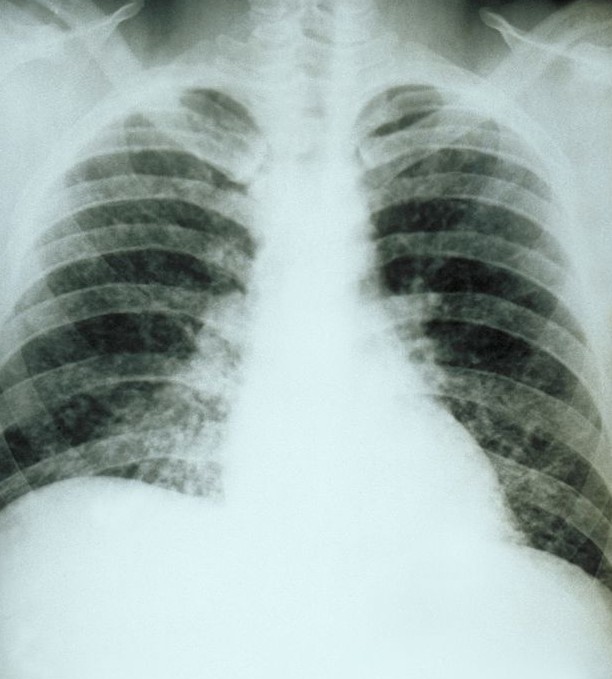
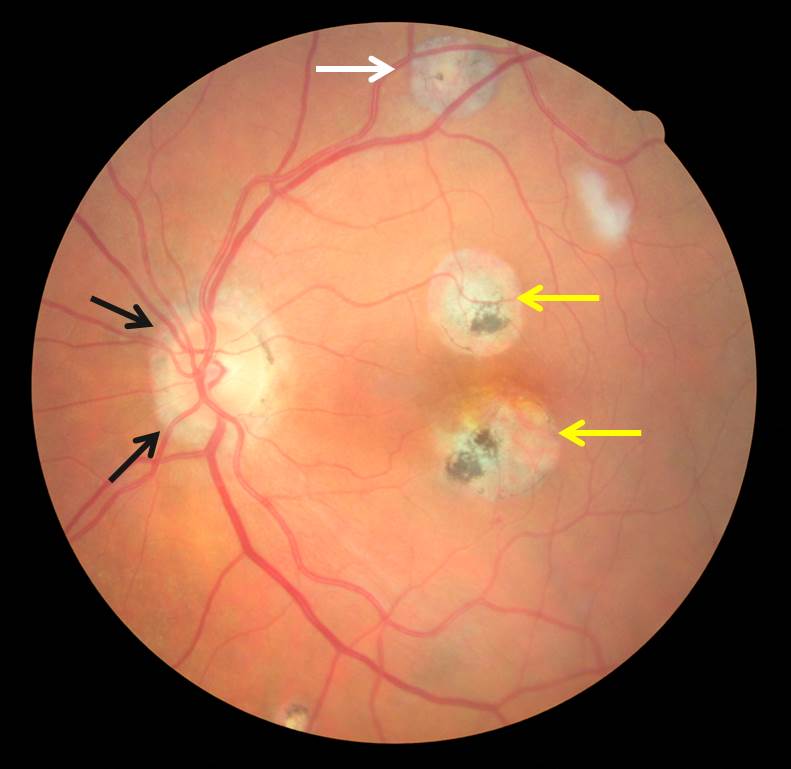
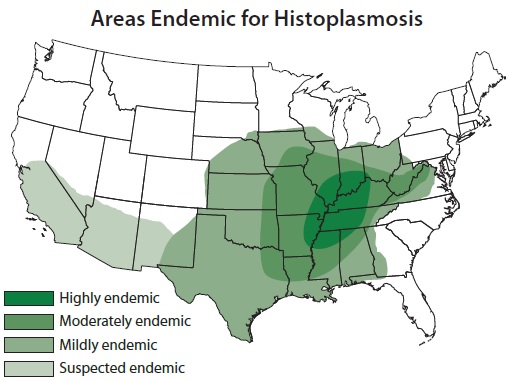 Any one, of any age, race, gender, or ethnicity is at risk for exposure and infection from the Histoplasmosis fungus. Those of us that reside in the Histo-Belt (Ohio and Mississippi River Valleys) are at a particularly high risk.
Any one, of any age, race, gender, or ethnicity is at risk for exposure and infection from the Histoplasmosis fungus. Those of us that reside in the Histo-Belt (Ohio and Mississippi River Valleys) are at a particularly high risk.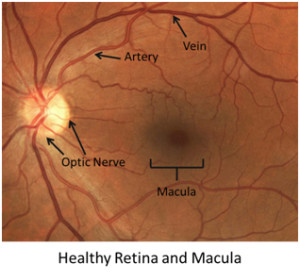

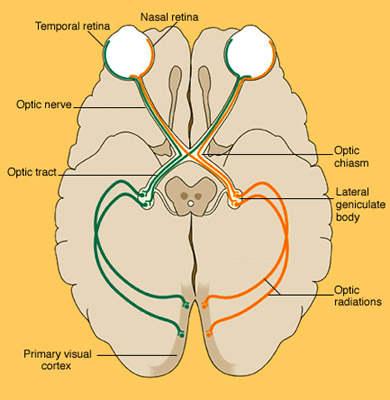 The eyes are obviously in the front, but they are a camera, nothing more. What actually “sees” is the occipital lobe at the back of the brain. The pictures from the eyes are sent via the optic nerve to the Lateral Geniculate Body (LGN) in brain for processing. After that, the processed signal is sent by optic radiations called the Meyer’s Loops to the Primary Visual Cortex of the occipital lobe which actually interprets the picture (diagram right).
The eyes are obviously in the front, but they are a camera, nothing more. What actually “sees” is the occipital lobe at the back of the brain. The pictures from the eyes are sent via the optic nerve to the Lateral Geniculate Body (LGN) in brain for processing. After that, the processed signal is sent by optic radiations called the Meyer’s Loops to the Primary Visual Cortex of the occipital lobe which actually interprets the picture (diagram right).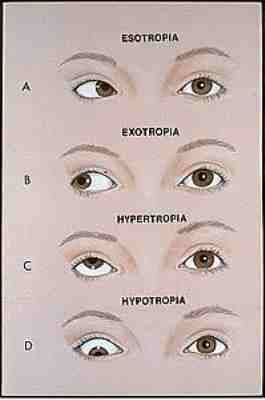 Strabismus is a condition that occurs when the eyes aren’t properly aligned with one another from birth. This results in one eye turning in, out, up or down with respect to the other eye. When the eyes are not working together properly, the brain is getting two different pictures from the eyes. This leads to double vision which the brain does not like. As a result, the brain will then decide to pick only one eye to develop properly and the input from the other turned eye will be ignored.
Strabismus is a condition that occurs when the eyes aren’t properly aligned with one another from birth. This results in one eye turning in, out, up or down with respect to the other eye. When the eyes are not working together properly, the brain is getting two different pictures from the eyes. This leads to double vision which the brain does not like. As a result, the brain will then decide to pick only one eye to develop properly and the input from the other turned eye will be ignored. Regardless of the cause, is important to identify and treat amblyopia as early in life as possible.
Regardless of the cause, is important to identify and treat amblyopia as early in life as possible.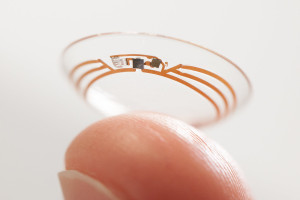 The first, and one you might have heard about, is a recent paring between Google and Alcon (eye care branch of the drug company Novartis).
The first, and one you might have heard about, is a recent paring between Google and Alcon (eye care branch of the drug company Novartis). Everyone who’s been to the eye doctor knows the dreaded “Puff of Air” but what that test is actually measuring is the pressure inside your eye.
Everyone who’s been to the eye doctor knows the dreaded “Puff of Air” but what that test is actually measuring is the pressure inside your eye.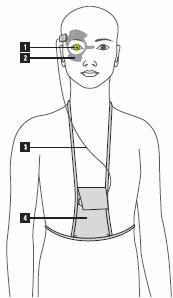 The Triggerfish is worn in one eye (1). A wireless antenna (2) is positioned around the eye to collect the data from the contact lens. Then a set of wires (3) sends data from the antenna to a recording device worn by the patient (4).
The Triggerfish is worn in one eye (1). A wireless antenna (2) is positioned around the eye to collect the data from the contact lens. Then a set of wires (3) sends data from the antenna to a recording device worn by the patient (4).
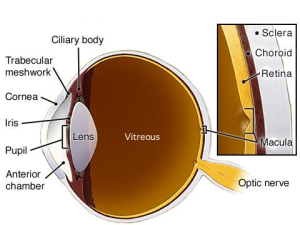
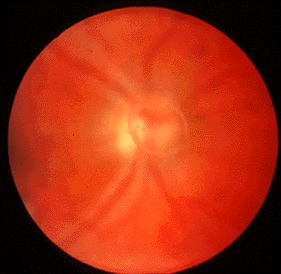 One specific type of floater that should always be investigated is something called a Posterior Vitreous Detachment (or PVD for short). PVDs occur as the liquefying jelly in our eye begins to collapse in on itself and peels away from the lining inside the eye, called the retina.
One specific type of floater that should always be investigated is something called a Posterior Vitreous Detachment (or PVD for short). PVDs occur as the liquefying jelly in our eye begins to collapse in on itself and peels away from the lining inside the eye, called the retina. Conductive Keratoplasty (pictured left) was a procedure that was done in the past by making thermal burns in a circular pattern on the cornea… this was pretty much a resounding failure and this procedure is rarely performed anymore.
Conductive Keratoplasty (pictured left) was a procedure that was done in the past by making thermal burns in a circular pattern on the cornea… this was pretty much a resounding failure and this procedure is rarely performed anymore.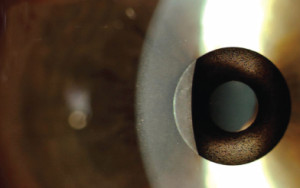 Corneal inlays are small pieces of plastic that are installed inside a pocket in the
Corneal inlays are small pieces of plastic that are installed inside a pocket in the 
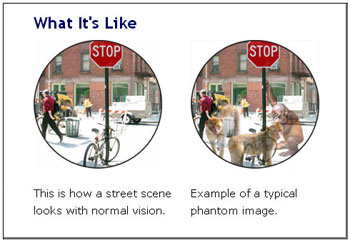 Visual hallucinations from Charles Bonnet Syndrome are quite varied but most often involve patterns, animals, people, or scenes and commonly fit into the individual’s actual surroundings. One characteristic of Charles Bonnet visions is that they are commonly “Lilliputian” hallucinations meaning everything and everyone look much smaller than they would normally appear. This trait of Charles Bonnet hallucinations results in individuals commonly seeing small pixie-like figures of varying colors and appearances.
Visual hallucinations from Charles Bonnet Syndrome are quite varied but most often involve patterns, animals, people, or scenes and commonly fit into the individual’s actual surroundings. One characteristic of Charles Bonnet visions is that they are commonly “Lilliputian” hallucinations meaning everything and everyone look much smaller than they would normally appear. This trait of Charles Bonnet hallucinations results in individuals commonly seeing small pixie-like figures of varying colors and appearances.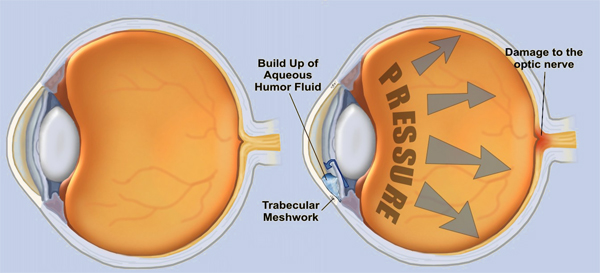


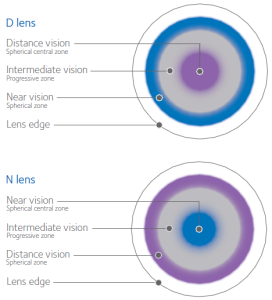 Instead, if you look at these lenses under a microscope they have concentric rings just like the rings on a dart board. Each ring of a bifocal contact lens is designed to focus for a different place: distance, intermediate or computer, and reading (see right). All the vision from all distances is focused by the contact onto the retina in the back of the eye and the retina sends that information to the brain.
Instead, if you look at these lenses under a microscope they have concentric rings just like the rings on a dart board. Each ring of a bifocal contact lens is designed to focus for a different place: distance, intermediate or computer, and reading (see right). All the vision from all distances is focused by the contact onto the retina in the back of the eye and the retina sends that information to the brain.