This will be a recurring series on Eye to the Future, where we will be looking into some of the more peculiar and odd eye conditions out there. Hopefully you will find these topics interesting, and if nothing else, maybe you can astonish your friends and family during Jeopardy!
 Yes!!! Amazingly enough…
Yes!!! Amazingly enough…
In addition to being a thinly veiled sexual euphemism made famous by rocker Ted Nugent, Cat Scratch Fever (or more accurately Cat Scratch Disease), is actually a relatively common condition that can cause some substantial eye related problems.
Cat Scratch Disease is a constellation of various systemic (and eye) symptoms that results from, logically, a cat’s scratch or bite. The underlying cause of Cat Scratch Fever is a bacterium called Bartonella (below, right) that was confirmed by Robert Debré in 1950 to be naturally occurring in cats and potentially infectious to humans. Bartonella is more commonly found in kittens/young cats and is most likely to occur in outdoor cats as fleas are the main method that Bartonella is spread within cat populations. Cats pick up this bug through fur cleaning of flea debris and foster this bacterium in their saliva which results in the spread to us through bites and scratches.
 When Bartonella is transmitted to humans it has a latent period of 1-3 weeks from the initial bite, but it is not uncommon for symptoms to only pop up 1-2 months later when the memory of the cat scratch has long faded. Cat Scratch Fever commonly presents with tender, swollen lymph nodes near the site of the scratch/bite and the afflicted also suffer from severe flu like symptoms with malaise, aches, fever, headache, and joint/muscle pain. In very severe cases, Bartonella can also can meningitis (infection/inflammation in the brain) or endocarditis (infection/inflammation in the heart).
When Bartonella is transmitted to humans it has a latent period of 1-3 weeks from the initial bite, but it is not uncommon for symptoms to only pop up 1-2 months later when the memory of the cat scratch has long faded. Cat Scratch Fever commonly presents with tender, swollen lymph nodes near the site of the scratch/bite and the afflicted also suffer from severe flu like symptoms with malaise, aches, fever, headache, and joint/muscle pain. In very severe cases, Bartonella can also can meningitis (infection/inflammation in the brain) or endocarditis (infection/inflammation in the heart).
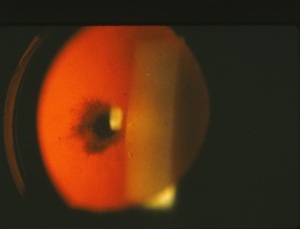
Pat ients with undiagnosed Cat Scratch Fever will often make a trip to their local eye doctor during this time because Cat Scratch Fever can cause a severe conjunctivitis (pink eye) and even very blurry vision from optic neuritis or neuroretinitis (inflammation of the optic nerve and retina). The optic nerve carries the signal from to the eye to the brain and inflammation of this nerve results in decreased vision (left photo is normal, right has an inflammed optic nerve and retina). The blurry vision from Cat Scratch Fever neuroretinitis is usually temporary.
ients with undiagnosed Cat Scratch Fever will often make a trip to their local eye doctor during this time because Cat Scratch Fever can cause a severe conjunctivitis (pink eye) and even very blurry vision from optic neuritis or neuroretinitis (inflammation of the optic nerve and retina). The optic nerve carries the signal from to the eye to the brain and inflammation of this nerve results in decreased vision (left photo is normal, right has an inflammed optic nerve and retina). The blurry vision from Cat Scratch Fever neuroretinitis is usually temporary.
Now, take a breath…. I know you are likely glancing at your friendly, family feline with a mixture of repulsion and horror… Fear not! Cat Scratch Fever from Bartonella is usually very benign and all symptoms typically abate within a couple weeks without any treatment. In fact, Bartonella infection is estimated to be quite under-diagnosed simply because severe complications are rare and symptoms are similar to the flu, and like the flu, improve on their own. If severe complications from Cat Scratch Disease do present, it is possible to shorten the length of symptoms through oral antibiotics, but the medical literature is conflicted on which medicines work best and how much treatment actually improves the condition.
I hope you’ve enjoyed this quick talk and the next time you hear Nugent’s risqué anthem playing on the radio… let it be a reminder to think twice before petting stray cats!!
– Nick Wolf, OD



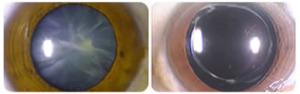 Cataract surgery permanently removes the clouded cataract and replaces our human lens with a crystal clear, man-made lens. Above is an advanced cataract on the left and the same eye after the cataract is removed and the implant positioned. It’s not hard to imagine the improvement this will have on vision. And the way in which this surgery has evolved as well as some newer implant options available is just…. awesome!
Cataract surgery permanently removes the clouded cataract and replaces our human lens with a crystal clear, man-made lens. Above is an advanced cataract on the left and the same eye after the cataract is removed and the implant positioned. It’s not hard to imagine the improvement this will have on vision. And the way in which this surgery has evolved as well as some newer implant options available is just…. awesome!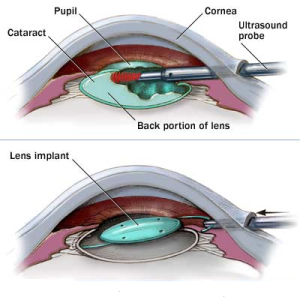 Cataract surgery is an outpatient procedure performed under general anesthesia which means you are awake but sedated. Cataract surgery is done one eye at a time (separated by one or more weeks of healing). During this procedure a cataract surgeon will make two small incisions in the cornea to allow instruments to be inserted into the eye. The crystalline lens sits in a thin membranous bag and to get to the lens, the front surface of the membranous bag is removed. In the past, the lens was removed whole, requiring a very large incision and a long recovery time. Nowadays, the surgeon uses an ultrasound probe to break up and remove the lens inside the eye. Now that the clouded lens is removed, a man made lens is put back in it in place allowing clear vision once again. The incisions are self-healing and no stitches are required. The entire surgery takes about 10 minutes.
Cataract surgery is an outpatient procedure performed under general anesthesia which means you are awake but sedated. Cataract surgery is done one eye at a time (separated by one or more weeks of healing). During this procedure a cataract surgeon will make two small incisions in the cornea to allow instruments to be inserted into the eye. The crystalline lens sits in a thin membranous bag and to get to the lens, the front surface of the membranous bag is removed. In the past, the lens was removed whole, requiring a very large incision and a long recovery time. Nowadays, the surgeon uses an ultrasound probe to break up and remove the lens inside the eye. Now that the clouded lens is removed, a man made lens is put back in it in place allowing clear vision once again. The incisions are self-healing and no stitches are required. The entire surgery takes about 10 minutes. When the cataract is removed from the eye, there is an opportunity for the surgeon to put any powered lens back in its place. Measurements are taken before the surgery to measure what powered lens is needed to correct for any underlying prescription like nearsighted, farsighted, or astigmatism. A lens is then chosen to correct for your individualized glasses prescription which results in most individuals being far less reliance on distance glasses after cataract surgery.
When the cataract is removed from the eye, there is an opportunity for the surgeon to put any powered lens back in its place. Measurements are taken before the surgery to measure what powered lens is needed to correct for any underlying prescription like nearsighted, farsighted, or astigmatism. A lens is then chosen to correct for your individualized glasses prescription which results in most individuals being far less reliance on distance glasses after cataract surgery.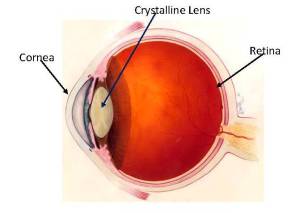 What is a cataract? Are there different types? Why does it form? What are the symptoms? What can you do about it? All good questions that eye doctors get asked on a near daily basis. Today on Eye to the Future we will seek to answer these and more as we demystify Cataracts.
What is a cataract? Are there different types? Why does it form? What are the symptoms? What can you do about it? All good questions that eye doctors get asked on a near daily basis. Today on Eye to the Future we will seek to answer these and more as we demystify Cataracts.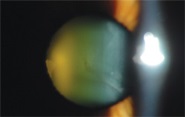

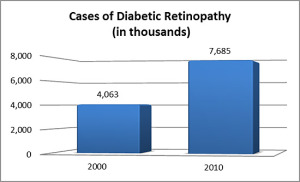 Even more concerning to eye care providers is that the incidence of ocular changes in Diabetic patients has increased by
Even more concerning to eye care providers is that the incidence of ocular changes in Diabetic patients has increased by 
 Each time you remove you contact lenses from the case you should dump the solution, rinse the case, and allow it to fully air dry before the next night’s use. We recommended this position for the case throughout the day (picture right). A closed case will not air dry and grow bacteria and a face up case will collect hairspray.
Each time you remove you contact lenses from the case you should dump the solution, rinse the case, and allow it to fully air dry before the next night’s use. We recommended this position for the case throughout the day (picture right). A closed case will not air dry and grow bacteria and a face up case will collect hairspray.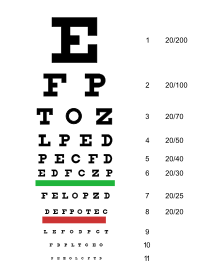 As eye doctors, we will often get asked the question…
As eye doctors, we will often get asked the question… The first person to understand the need for a standardized way of measuring vision was a German ophthalmologist named Heinrich Keuchler. Around 1842, Keuchler created the very first visual acuity chart. Actually, he created 3 different ones to prevent his patients from memorizing the letters… you all know who you are.
The first person to understand the need for a standardized way of measuring vision was a German ophthalmologist named Heinrich Keuchler. Around 1842, Keuchler created the very first visual acuity chart. Actually, he created 3 different ones to prevent his patients from memorizing the letters… you all know who you are.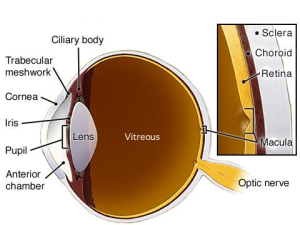




 Diagnosis of color deficiency is very straightforward during a normal eye exam. This is done by using colored plates with dots in various patterns to spell out letters, numbers, lines, or shapes. These color plates (like the Ishihara plates at right) use specific colors chosen to be difficult for color deficient individuals to tell the difference. As a result, these individuals have trouble identifying the number or numbers on the plate, but for a color normal individual this will be very easy.
Diagnosis of color deficiency is very straightforward during a normal eye exam. This is done by using colored plates with dots in various patterns to spell out letters, numbers, lines, or shapes. These color plates (like the Ishihara plates at right) use specific colors chosen to be difficult for color deficient individuals to tell the difference. As a result, these individuals have trouble identifying the number or numbers on the plate, but for a color normal individual this will be very easy. The benefits of eye dilation don’t stop with the eye. The interior of the eye is unique in that is it the only place in the body where nerve tissue and blood vessels can be viewed without any advanced procedures or expensive testing. This allows your eye doctor a perfect opportunity to use the information gleaned from your dilated exam to identify problems and conditions elsewhere in the body. There are quite literally hundreds of systemic conditions (
The benefits of eye dilation don’t stop with the eye. The interior of the eye is unique in that is it the only place in the body where nerve tissue and blood vessels can be viewed without any advanced procedures or expensive testing. This allows your eye doctor a perfect opportunity to use the information gleaned from your dilated exam to identify problems and conditions elsewhere in the body. There are quite literally hundreds of systemic conditions ( A friendly gentlemen came in to see me today with a very angry eye and reported that he had been working on his son’s car earlier in the week and his eye has been red and scratchy every since. As I was preparing to drill out the large hunk of rusted metal (left), it dawned on me, October is Eye Injury Prevention Month!
A friendly gentlemen came in to see me today with a very angry eye and reported that he had been working on his son’s car earlier in the week and his eye has been red and scratchy every since. As I was preparing to drill out the large hunk of rusted metal (left), it dawned on me, October is Eye Injury Prevention Month! Workshop
Workshop