 With school back in full swing, Precision Family Eye Care and the Eye to the Future blog want to take a moment this week to impress upon all parents the importance of getting routine vision exams for all school age children.
With school back in full swing, Precision Family Eye Care and the Eye to the Future blog want to take a moment this week to impress upon all parents the importance of getting routine vision exams for all school age children.
School and Pediatrician screenings are simply not adequate, and unlike adults, children can’t articulate their vision problems because they don’t understand that the way they see the world isn’t “normal.” Uncorrected prescription (like nearsighted, farsighted, and astigmatism) as well as eye alignment and focusing problems, and even ocular diseases can all inhibit the ability of your child to use their eyes properly. This leads to disrupted vision and potentially vision threatening conditions being simply overlooked or even causing learning problems and leading to a diagnosis of LD (Learning Disorders), ADHD or even dyslexia.
The learning environment today is flush with visual tasks: smart boards, iPads, digital learning, computer work, homework, test taking, etc. It shouldn’t surprise us then, that learning experts estimate that roughly 80% of all learning is dependent upon the sense of sight and unfortunately, at least 25% of school aged children have a visual impairment that may prevent a child from reaching their full academic potential.
Please make sure that your child has the proper tools for academic success this year by scheduling a comprehensive exam with your eye doctor today!



 We hope you have enjoyed this long answer to a short question. Next time on Eye to the Future, we will be discussing polarized lens. How they work, how they’re made, and why they are so, so useful for clarity and vision.
We hope you have enjoyed this long answer to a short question. Next time on Eye to the Future, we will be discussing polarized lens. How they work, how they’re made, and why they are so, so useful for clarity and vision.
 Seborrheic Blepharitis (picture right) – This chronic condition occurs on the sensitive eye lid skin at the level of and continuing up or down the lid from the lash line; although it is more common on the upper eyelid. This condition is a subtype of dermatitis that causes malfunction of sebaceous glands (oil producing glands) on the eye lid skin and often occurs in conjunction with dermatitis elsewhere on the head and face. This condition occurs secondary to hypersensitivity to the presence of bacteria or fungus, genetics, or environmental or health factors. Regardless of the underlying cause, this condition results in flaking, cracking, crusting, or dandruff on the eyelid skin along with crusting of the skin or lashes and erythematosus (redness and inflammation) of the lid. The main treatment for this condition is prescription antibiotic and/or steroid creams.
Seborrheic Blepharitis (picture right) – This chronic condition occurs on the sensitive eye lid skin at the level of and continuing up or down the lid from the lash line; although it is more common on the upper eyelid. This condition is a subtype of dermatitis that causes malfunction of sebaceous glands (oil producing glands) on the eye lid skin and often occurs in conjunction with dermatitis elsewhere on the head and face. This condition occurs secondary to hypersensitivity to the presence of bacteria or fungus, genetics, or environmental or health factors. Regardless of the underlying cause, this condition results in flaking, cracking, crusting, or dandruff on the eyelid skin along with crusting of the skin or lashes and erythematosus (redness and inflammation) of the lid. The main treatment for this condition is prescription antibiotic and/or steroid creams. Bacterial Blepharitis – This type of blepharitis occurs from a either an acute or a chronic bacterial infection of eyelid margin at the base of the eyelashes. Typically this infection comes from gram-positive Staphylococcal or simply “Staph” bacterial with the most common culprit in this family being Staph Aureus (electron micrograph image right). These Staph bacterial are extremely common on the human skin and in the eyes, but inflammation or infection comes from over population or hyper sensitivity to these bacterium. In acute cases, over population of bacterial causes a sudden, active, and contagious infection of the eyelids with redness, moderate to severe crusting and matting. This infection can also cause a concurrent infection on the white of the eye called conjunctivitis (“pink eye”) and in severe cases a keratitis which is an infection on the cornea.
Bacterial Blepharitis – This type of blepharitis occurs from a either an acute or a chronic bacterial infection of eyelid margin at the base of the eyelashes. Typically this infection comes from gram-positive Staphylococcal or simply “Staph” bacterial with the most common culprit in this family being Staph Aureus (electron micrograph image right). These Staph bacterial are extremely common on the human skin and in the eyes, but inflammation or infection comes from over population or hyper sensitivity to these bacterium. In acute cases, over population of bacterial causes a sudden, active, and contagious infection of the eyelids with redness, moderate to severe crusting and matting. This infection can also cause a concurrent infection on the white of the eye called conjunctivitis (“pink eye”) and in severe cases a keratitis which is an infection on the cornea. 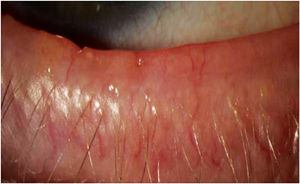 Although acute bacterial blepharitis is common, since this bacterial is so commonly found on the skin surface it is more common to see a chronic long term hypersensitivity to the offending bacterium. Chronic bacterial blepharitis causes less overt symptoms but far worse, long term, and irreversible complications including crusting, thickening, ulceration, scarring of the eyelids, and permanent loss of lashes (seen at left).
Although acute bacterial blepharitis is common, since this bacterial is so commonly found on the skin surface it is more common to see a chronic long term hypersensitivity to the offending bacterium. Chronic bacterial blepharitis causes less overt symptoms but far worse, long term, and irreversible complications including crusting, thickening, ulceration, scarring of the eyelids, and permanent loss of lashes (seen at left).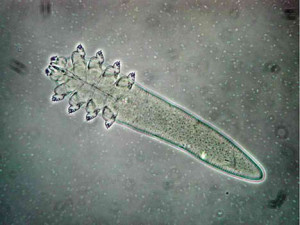 Demodex Blepharitis – I promised you parasites! Like Staphylococcal bacteria, Demodex (pictured at right) are also a ubiquitous and largely benign resident of the human skin. Demodex are a parasitic mite that spends its life living inside the hair follicles of ALL mammals. You are probably familiar with mange in dogs? Yep, that’s demodex (infected follicle at right). The prevalence of eyelash demodex in humans increases with age – from 85% prevalence by age 60 to nearly 100% of humans by age 70, but it is commonly found in patients of all age ranges. Luckily for us, the
Demodex Blepharitis – I promised you parasites! Like Staphylococcal bacteria, Demodex (pictured at right) are also a ubiquitous and largely benign resident of the human skin. Demodex are a parasitic mite that spends its life living inside the hair follicles of ALL mammals. You are probably familiar with mange in dogs? Yep, that’s demodex (infected follicle at right). The prevalence of eyelash demodex in humans increases with age – from 85% prevalence by age 60 to nearly 100% of humans by age 70, but it is commonly found in patients of all age ranges. Luckily for us, the 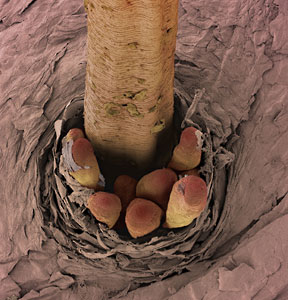 vast majority of the time, this parasitic relationship occurs without any problems or symptoms.
vast majority of the time, this parasitic relationship occurs without any problems or symptoms.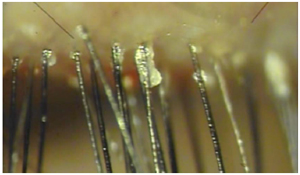 ich are very effective at lowing the overall population. It is very common, however, for the symptoms to return as the mites multiply over time. Therefore, a daily eyelid cleaning
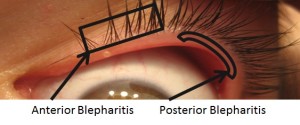
ich are very effective at lowing the overall population. It is very common, however, for the symptoms to return as the mites multiply over time. Therefore, a daily eyelid cleaning This condition is also known as Meibomian Gland Dysfunction or simply MGD (no, not the frosty adult beverage). This form of lid inflammation occurs at the inner edge of the eyelid next to the eyeball where the meibomian (or oil producing) glands are located. As previously mentioned, these oil glands produce a very important oil that coats over the watery layer of the tears with every blink. Without proper amounts or quality of this oil the tear film becomes unstable and evaporates too quickly to keep the eye properly wetted. As a result, Posterior Blepharitis is the leading underlying cause of evaporative Dry Eye Syndrome (DES). Inflammation on this part of the eyelid results in these important oil glands clogging and become “capped” or “plugged up” as is shown above. As these oil glands get clogged, the clear oil they typically produce turns to very thick almost che
This condition is also known as Meibomian Gland Dysfunction or simply MGD (no, not the frosty adult beverage). This form of lid inflammation occurs at the inner edge of the eyelid next to the eyeball where the meibomian (or oil producing) glands are located. As previously mentioned, these oil glands produce a very important oil that coats over the watery layer of the tears with every blink. Without proper amounts or quality of this oil the tear film becomes unstable and evaporates too quickly to keep the eye properly wetted. As a result, Posterior Blepharitis is the leading underlying cause of evaporative Dry Eye Syndrome (DES). Inflammation on this part of the eyelid results in these important oil glands clogging and become “capped” or “plugged up” as is shown above. As these oil glands get clogged, the clear oil they typically produce turns to very thick almost che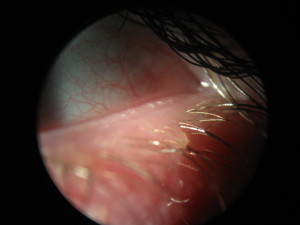 esy oil (shown above) along with foamy or frothy tears (right). In addition to problems with the oily layer, the natural bacterial in our tears also tends to get trapped in the clogged glands and can cause an infection of that gland; this is how stys are formed.
esy oil (shown above) along with foamy or frothy tears (right). In addition to problems with the oily layer, the natural bacterial in our tears also tends to get trapped in the clogged glands and can cause an infection of that gland; this is how stys are formed.
 aritis
aritis
 Chris Sowder, our office administrator, brings to our practice nearly 20 years of experience. Chris has an Associate of Science degree from Indiana School of Optometry’s optician/technician program. Following school she was an assistant retail manager at a large optical chain, providing her with customer service and optician/dispensing experience. Chris then made a career move to the medical side of optometry as a lead ophthalmic technician for Bennett and Bloom Eye Centers. This experience taught her the importance of early treatment for ocular disease. Most recently, Chris has worked for a busy private practice where she was cross-trained in every department. It has always been Chris’s goal to maximize her college degree and work as an office manager of a locally owned, state-of-the-art Optometry practice. The road she has taken to get here gives her every advantage helping her patients get the most out of their eye care needs. This born and raised Hoosier spent a few years in Bloomington and Indianapolis, but is now proud to call her hometown of Pekin, Indiana home once again. Chris is married and has three school-aged children to keep her busy in her time away from work.
Chris Sowder, our office administrator, brings to our practice nearly 20 years of experience. Chris has an Associate of Science degree from Indiana School of Optometry’s optician/technician program. Following school she was an assistant retail manager at a large optical chain, providing her with customer service and optician/dispensing experience. Chris then made a career move to the medical side of optometry as a lead ophthalmic technician for Bennett and Bloom Eye Centers. This experience taught her the importance of early treatment for ocular disease. Most recently, Chris has worked for a busy private practice where she was cross-trained in every department. It has always been Chris’s goal to maximize her college degree and work as an office manager of a locally owned, state-of-the-art Optometry practice. The road she has taken to get here gives her every advantage helping her patients get the most out of their eye care needs. This born and raised Hoosier spent a few years in Bloomington and Indianapolis, but is now proud to call her hometown of Pekin, Indiana home once again. Chris is married and has three school-aged children to keep her busy in her time away from work.