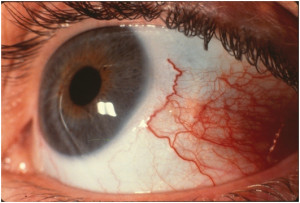
- Abrasions usually trauma related
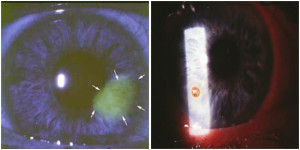
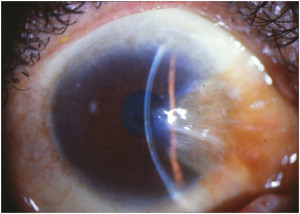
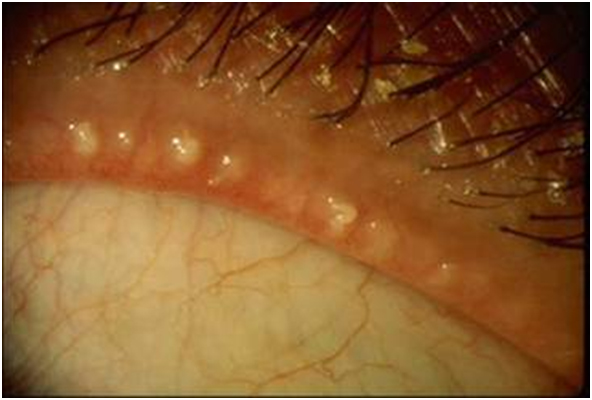
- Foreign body usually metal, glass, or organic material
Management
- Removal of foreign body, antibiotic coverage, cycloplegic if needed, and bandage contact lens for comfort
- Follow daily until wound heals
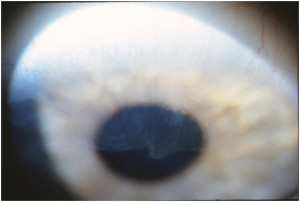
- Consider hypertonic (salt) solutions or ointment to decrease risk of recurrent epithelial erosions