Statistics and Associations
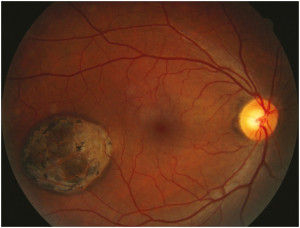
- Relatively low risk of melanoma; approximately 4 in 1000
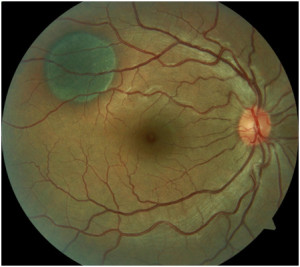
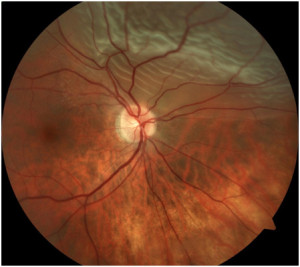
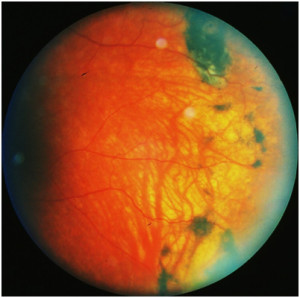
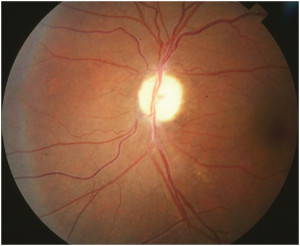
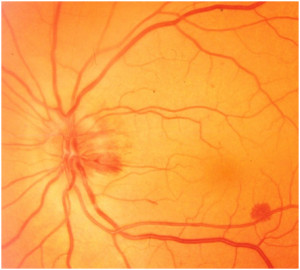
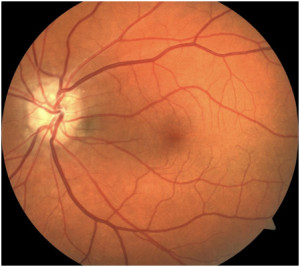
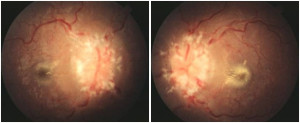
- Suspicious lesions include growth (after puberty), significant elevation, underlying fluid, overlying orange pigment, close proximity to optic nerve and resultant visual symptoms
Management
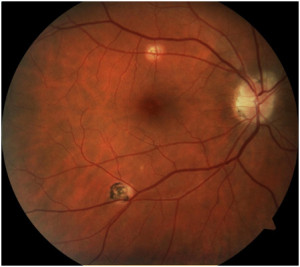
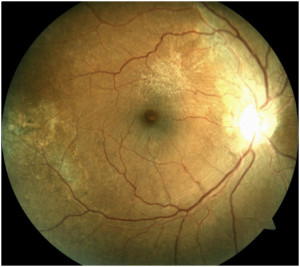
- Photography for baseline
- Suspicious Nevi should be followed with serial photography to detect any changes