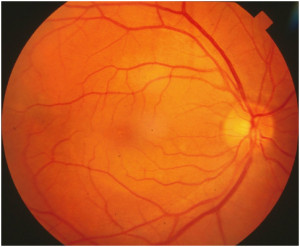
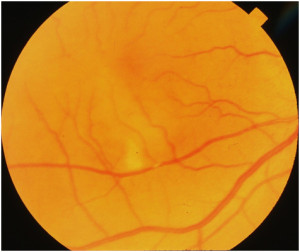
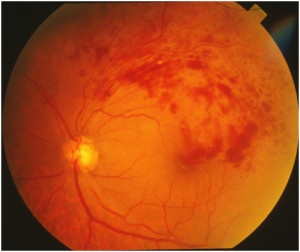
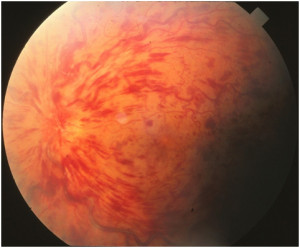
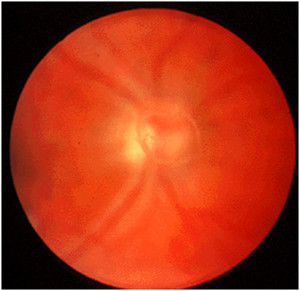
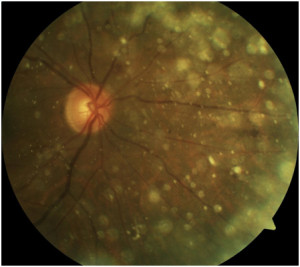
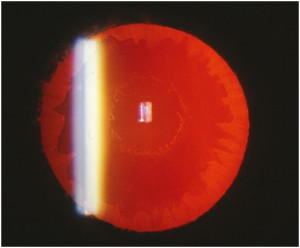
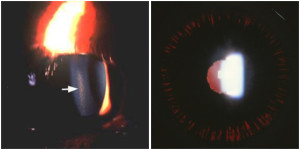
- Leakage of fluid leading to a blister in the subretinal space
- Commonly associated with type A personality and recent stress
- Most common in males (10:1), more common in whites (rare in blacks)
- 45% recurrence rate within one year
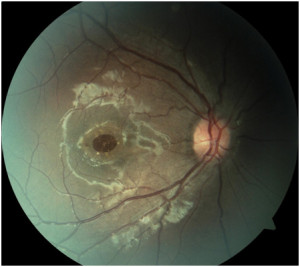
- 5% develop new blood vessel growth under the retina (SRNVM)
- 95% end up with vision better than 20/40
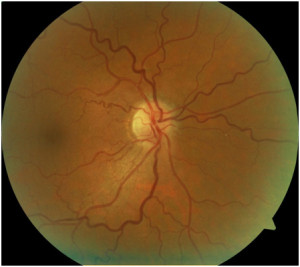
Management
- Amsler grid for daily monitoring
- No treatment necessary (usually resolves within 3 months)