Contact Lenses for more than Vision
As optometrists, we fit contact lenses daily. While new contact lens materials and designs have greatly increased the comfort and vision of our contact lens patients, we couldn’t help but wonder if contact lenses had additional diagnostic potential…
With that backdrop, some recent announcements and advancements in contact lens technology has got us very, very excited. Several different companies are now looking at ways of incorporating recent technological breakthroughs into contact lenses for the purposes of disease monitoring.
Today on Eye to the Future, we will delve into two contact lenses of the future.
Google/Alcon’s Blood Sugar Monitoring Lens
 The first, and one you might have heard about, is a recent paring between Google and Alcon (eye care branch of the drug company Novartis).
The first, and one you might have heard about, is a recent paring between Google and Alcon (eye care branch of the drug company Novartis).
While I personally cannot wait for a self driving car, the geniuses over a Google have equally excited our profession with their recent announcement to use their expertise to develop a contact lens that monitors blood sugar for diabetic patients.
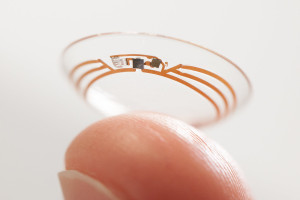
This contact lens (pictured at left) would contain micro sensors to measure the blood sugar levels in the tears as well as a radio antenna thinner than a human hair. The data is then transmitted from the antenna to a smart phone app to allow the continuous monitoring of blood sugar.
With the epidemic of diabetes in this country, this non-invasive contact lens of the future could revolutionize the way patients monitor their blood glucose levels. In addition to the easy of measurements and lack of finger sticks, this information would be enormously helpful for primary care doctors and endocrinologists in developing specific treatments plans depending on how blood sugar levels change throughout the day.
The Triggerfish by Sensimed
 Everyone who’s been to the eye doctor knows the dreaded “Puff of Air” but what that test is actually measuring is the pressure inside your eye.
Everyone who’s been to the eye doctor knows the dreaded “Puff of Air” but what that test is actually measuring is the pressure inside your eye.
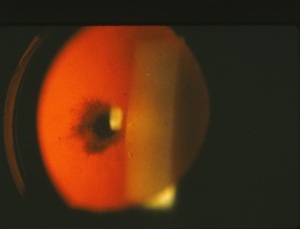
The Swiss company Sensimed has developed a wearable tech heavy contact lens called the Triggerfish. This contact lens of the future (right) was designed for the sole purpose of continuously measuring eye pressure over a 24 hour period.
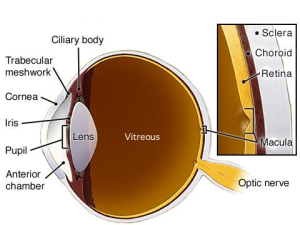
Eye pressure, or intraocular pressure (IOP), is an important factor in the diagnosis of Glaucoma and even more important in determining the effectiveness of a Glaucoma treatment. The problem with eye pressure is that it fluctuates quite a bit throughout the day, as much as 50% or more in glaucoma patients.
IOP tends to be lowest in the afternoon or early evening when many people get eye exams. This can give us a false sense of security that the eye pressure is “normal”. Even worse, the IOP also tends to be highest when we can’t record it, usually the very early morning hours when most of us are just waking up or enjoying our morning cup of coffee.
Having a graph of the high and low points with this non-invasive testing would allow eye doctors the ability to choose specific treatments that are most effective when the eye pressure tends to be highest.
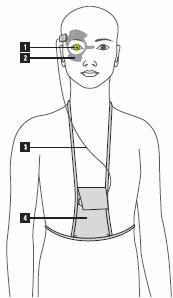 The Triggerfish is worn in one eye (1). A wireless antenna (2) is positioned around the eye to collect the data from the contact lens. Then a set of wires (3) sends data from the antenna to a recording device worn by the patient (4).
The Triggerfish is worn in one eye (1). A wireless antenna (2) is positioned around the eye to collect the data from the contact lens. Then a set of wires (3) sends data from the antenna to a recording device worn by the patient (4).
The patient is fit with the contact lens and antenna in office and simply wears this device as well as a monitoring pack for 24 hours before returning to the doctor where the data is downloaded and analyzed. This is very similar to heart monitors often used by primary care doctors and cardiologists to record a patients cardiac measurements outside the office setting.
This lens is currently going through studies in the US to determine its safety and effectiveness, but is already in full use overseas.
For additional information on the Triggerfish diagnostic contact lens, please visit the Sensimed website.
We hope you have enjoyed this little overview of the some contact lenses of the future. If you have any questions, as always, please contact us and ask.




 One specific type of floater that should always be investigated is something called a Posterior Vitreous Detachment (or PVD for short). PVDs occur as the liquefying jelly in our eye begins to collapse in on itself and peels away from the lining inside the eye, called the retina.
One specific type of floater that should always be investigated is something called a Posterior Vitreous Detachment (or PVD for short). PVDs occur as the liquefying jelly in our eye begins to collapse in on itself and peels away from the lining inside the eye, called the retina. Conductive Keratoplasty (pictured left) was a procedure that was done in the past by making thermal burns in a circular pattern on the cornea… this was pretty much a resounding failure and this procedure is rarely performed anymore.
Conductive Keratoplasty (pictured left) was a procedure that was done in the past by making thermal burns in a circular pattern on the cornea… this was pretty much a resounding failure and this procedure is rarely performed anymore.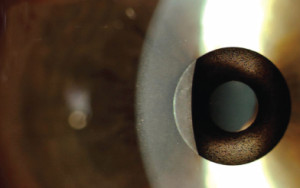 Corneal inlays are small pieces of plastic that are installed inside a pocket in the
Corneal inlays are small pieces of plastic that are installed inside a pocket in the 
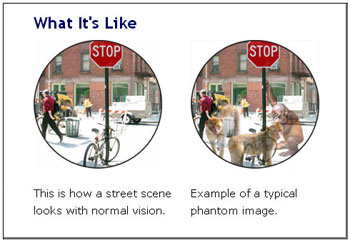 Visual hallucinations from Charles Bonnet Syndrome are quite varied but most often involve patterns, animals, people, or scenes and commonly fit into the individual’s actual surroundings. One characteristic of Charles Bonnet visions is that they are commonly “Lilliputian” hallucinations meaning everything and everyone look much smaller than they would normally appear. This trait of Charles Bonnet hallucinations results in individuals commonly seeing small pixie-like figures of varying colors and appearances.
Visual hallucinations from Charles Bonnet Syndrome are quite varied but most often involve patterns, animals, people, or scenes and commonly fit into the individual’s actual surroundings. One characteristic of Charles Bonnet visions is that they are commonly “Lilliputian” hallucinations meaning everything and everyone look much smaller than they would normally appear. This trait of Charles Bonnet hallucinations results in individuals commonly seeing small pixie-like figures of varying colors and appearances.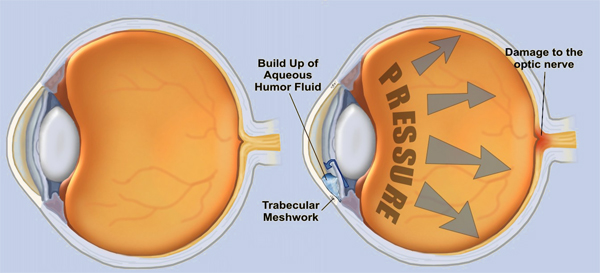


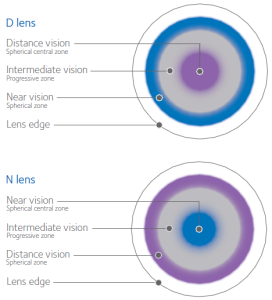 Instead, if you look at these lenses under a microscope they have concentric rings just like the rings on a dart board. Each ring of a bifocal contact lens is designed to focus for a different place: distance, intermediate or computer, and reading (see right). All the vision from all distances is focused by the contact onto the retina in the back of the eye and the retina sends that information to the brain.
Instead, if you look at these lenses under a microscope they have concentric rings just like the rings on a dart board. Each ring of a bifocal contact lens is designed to focus for a different place: distance, intermediate or computer, and reading (see right). All the vision from all distances is focused by the contact onto the retina in the back of the eye and the retina sends that information to the brain. Yes!!! Amazingly enough…
Yes!!! Amazingly enough…
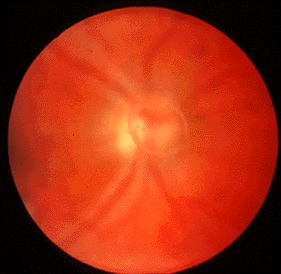
 ients with undiagnosed Cat Scratch Fever will often make a trip to their local eye doctor during this time because Cat Scratch Fever can cause a severe conjunctivitis (pink eye) and even very blurry vision from optic neuritis or neuroretinitis (inflammation of the optic nerve and retina). The optic nerve carries the signal from to the eye to the brain and inflammation of this nerve results in decreased vision (left photo is normal, right has an inflammed optic nerve and retina). The blurry vision from Cat Scratch Fever neuroretinitis is usually temporary.
ients with undiagnosed Cat Scratch Fever will often make a trip to their local eye doctor during this time because Cat Scratch Fever can cause a severe conjunctivitis (pink eye) and even very blurry vision from optic neuritis or neuroretinitis (inflammation of the optic nerve and retina). The optic nerve carries the signal from to the eye to the brain and inflammation of this nerve results in decreased vision (left photo is normal, right has an inflammed optic nerve and retina). The blurry vision from Cat Scratch Fever neuroretinitis is usually temporary.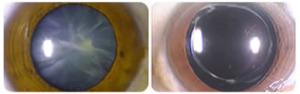 Cataract surgery permanently removes the clouded cataract and replaces our human lens with a crystal clear, man-made lens. Above is an advanced cataract on the left and the same eye after the cataract is removed and the implant positioned. It’s not hard to imagine the improvement this will have on vision. And the way in which this surgery has evolved as well as some newer implant options available is just…. awesome!
Cataract surgery permanently removes the clouded cataract and replaces our human lens with a crystal clear, man-made lens. Above is an advanced cataract on the left and the same eye after the cataract is removed and the implant positioned. It’s not hard to imagine the improvement this will have on vision. And the way in which this surgery has evolved as well as some newer implant options available is just…. awesome!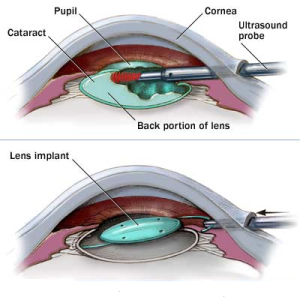 Cataract surgery is an outpatient procedure performed under general anesthesia which means you are awake but sedated. Cataract surgery is done one eye at a time (separated by one or more weeks of healing). During this procedure a cataract surgeon will make two small incisions in the cornea to allow instruments to be inserted into the eye. The crystalline lens sits in a thin membranous bag and to get to the lens, the front surface of the membranous bag is removed. In the past, the lens was removed whole, requiring a very large incision and a long recovery time. Nowadays, the surgeon uses an ultrasound probe to break up and remove the lens inside the eye. Now that the clouded lens is removed, a man made lens is put back in it in place allowing clear vision once again. The incisions are self-healing and no stitches are required. The entire surgery takes about 10 minutes.
Cataract surgery is an outpatient procedure performed under general anesthesia which means you are awake but sedated. Cataract surgery is done one eye at a time (separated by one or more weeks of healing). During this procedure a cataract surgeon will make two small incisions in the cornea to allow instruments to be inserted into the eye. The crystalline lens sits in a thin membranous bag and to get to the lens, the front surface of the membranous bag is removed. In the past, the lens was removed whole, requiring a very large incision and a long recovery time. Nowadays, the surgeon uses an ultrasound probe to break up and remove the lens inside the eye. Now that the clouded lens is removed, a man made lens is put back in it in place allowing clear vision once again. The incisions are self-healing and no stitches are required. The entire surgery takes about 10 minutes. When the cataract is removed from the eye, there is an opportunity for the surgeon to put any powered lens back in its place. Measurements are taken before the surgery to measure what powered lens is needed to correct for any underlying prescription like nearsighted, farsighted, or astigmatism. A lens is then chosen to correct for your individualized glasses prescription which results in most individuals being far less reliance on distance glasses after cataract surgery.
When the cataract is removed from the eye, there is an opportunity for the surgeon to put any powered lens back in its place. Measurements are taken before the surgery to measure what powered lens is needed to correct for any underlying prescription like nearsighted, farsighted, or astigmatism. A lens is then chosen to correct for your individualized glasses prescription which results in most individuals being far less reliance on distance glasses after cataract surgery.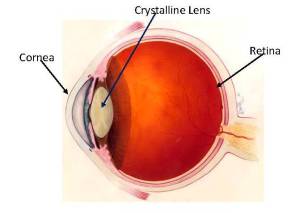 What is a cataract? Are there different types? Why does it form? What are the symptoms? What can you do about it? All good questions that eye doctors get asked on a near daily basis. Today on Eye to the Future we will seek to answer these and more as we demystify Cataracts.
What is a cataract? Are there different types? Why does it form? What are the symptoms? What can you do about it? All good questions that eye doctors get asked on a near daily basis. Today on Eye to the Future we will seek to answer these and more as we demystify Cataracts.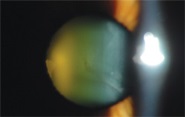

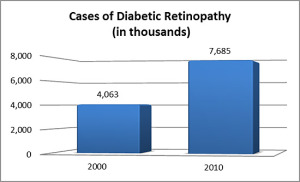 Even more concerning to eye care providers is that the incidence of ocular changes in Diabetic patients has increased by
Even more concerning to eye care providers is that the incidence of ocular changes in Diabetic patients has increased by