Every contact lens wearer remembers their first experience with contact lenses- the excitement, the freedom from glasses. However, what is often forgotten is the tips, training, and recommendations given by the eye care provider. Today we will be doing a quick refresher on proper contact lens care.
Every contact lens wearer remembers their first experience with contact lenses- the excitement, the freedom from glasses. However, what is often forgotten is the tips, training, and recommendations given by the eye care provider. Today we will be doing a quick refresher on proper contact lens care.
Why is this even necessary?
Simply put, getting into the habit of proper contact lens care goes a very, very long way to ensuring you have a comfortable and healthy experience while wearing these medical devices.
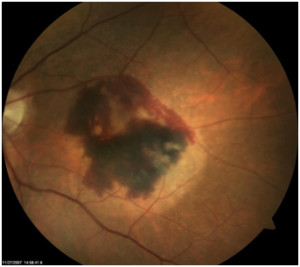
I could put up picture after picture of the horrible things I’ve personally seen that were caused by contact lens misuse and abuse. However, let’s just say that complications from contact lenses are a leading cause of preventable blindness in US. If you’re inclined to horrible graphic pictures, type “contact lens corneal ulcer” into google images…
We don’t like seeing these complications so here are the recommendations for contact lens care that we try to instill at Precision Family Eye Care:
- Always wash and dry your hands before handling the contacts and avoid moisturizing soaps that will leave a film.
- Contacts come first – put in the contacts before applying makeup or creams to prevent cosmetics from adhering to the lens.
- Use only the multipurpose cleaning solutions recommended by your doctor. Eye drops, saline, or tap water will not disinfect your contacts and will cause a problem.
- Please rub to clean the contacts. Rinsing and soaking is not sufficient. A simple cleaning will go a long way to keeping the lenses fresh and clean.
- Never, ever reuse or top off contact lenses solution!! This cannot be overstated.
 Each time you remove you contact lenses from the case you should dump the solution, rinse the case, and allow it to fully air dry before the next night’s use. We recommended this position for the case throughout the day (picture right). A closed case will not air dry and grow bacteria and a face up case will collect hairspray.
Each time you remove you contact lenses from the case you should dump the solution, rinse the case, and allow it to fully air dry before the next night’s use. We recommended this position for the case throughout the day (picture right). A closed case will not air dry and grow bacteria and a face up case will collect hairspray.- Even with perfect care, a case will begin to grow bacteria over time. Cases should be boiled or replaced at least every 3 months.
- Please do not wear your contacts while swimming. Chlorine is very rough on contacts and there are plenty of critters in both hot tubs and fresh water that would love to start growing on your eyes.
- Sleeping over night in contacts increases your chances of getting an eye infection by 15 times! If you absolutely must, please let you eye care provider know so they can prescribe lenses made for overnight wear.
- Contact lenses carry a FDA approved wearing time for a reason. If you use eye irritation as the judge of when you change your lenses, you are already doing microscopic damage to the surface of your eye that could lead to an infection.
If you notice pain, redness, light sensitivity, blurry vision, or irritation remove your lenses and contact you eye care provider.
Please follow these contact lens care recommendations. Your eyes are too important to take a chance on!
Click here to see the FDA recommendations on contact lens care and potential risks
– Nick Wolf, OD



 As eye doctors, we will often get asked the question…
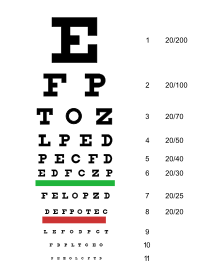
As eye doctors, we will often get asked the question… The first person to understand the need for a standardized way of measuring vision was a German ophthalmologist named Heinrich Keuchler. Around 1842, Keuchler created the very first visual acuity chart. Actually, he created 3 different ones to prevent his patients from memorizing the letters… you all know who you are.
The first person to understand the need for a standardized way of measuring vision was a German ophthalmologist named Heinrich Keuchler. Around 1842, Keuchler created the very first visual acuity chart. Actually, he created 3 different ones to prevent his patients from memorizing the letters… you all know who you are.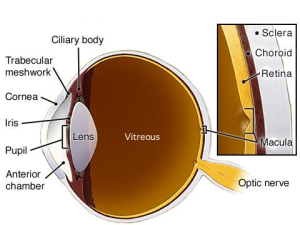




 Diagnosis of color deficiency is very straightforward during a normal eye exam. This is done by using colored plates with dots in various patterns to spell out letters, numbers, lines, or shapes. These color plates (like the Ishihara plates at right) use specific colors chosen to be difficult for color deficient individuals to tell the difference. As a result, these individuals have trouble identifying the number or numbers on the plate, but for a color normal individual this will be very easy.
Diagnosis of color deficiency is very straightforward during a normal eye exam. This is done by using colored plates with dots in various patterns to spell out letters, numbers, lines, or shapes. These color plates (like the Ishihara plates at right) use specific colors chosen to be difficult for color deficient individuals to tell the difference. As a result, these individuals have trouble identifying the number or numbers on the plate, but for a color normal individual this will be very easy. The benefits of eye dilation don’t stop with the eye. The interior of the eye is unique in that is it the only place in the body where nerve tissue and blood vessels can be viewed without any advanced procedures or expensive testing. This allows your eye doctor a perfect opportunity to use the information gleaned from your dilated exam to identify problems and conditions elsewhere in the body. There are quite literally hundreds of systemic conditions (
The benefits of eye dilation don’t stop with the eye. The interior of the eye is unique in that is it the only place in the body where nerve tissue and blood vessels can be viewed without any advanced procedures or expensive testing. This allows your eye doctor a perfect opportunity to use the information gleaned from your dilated exam to identify problems and conditions elsewhere in the body. There are quite literally hundreds of systemic conditions ( A friendly gentlemen came in to see me today with a very angry eye and reported that he had been working on his son’s car earlier in the week and his eye has been red and scratchy every since. As I was preparing to drill out the large hunk of rusted metal (left), it dawned on me, October is Eye Injury Prevention Month!
A friendly gentlemen came in to see me today with a very angry eye and reported that he had been working on his son’s car earlier in the week and his eye has been red and scratchy every since. As I was preparing to drill out the large hunk of rusted metal (left), it dawned on me, October is Eye Injury Prevention Month! Workshop
Workshop
 We hope you have enjoyed this long answer to a short question. Next time on Eye to the Future, we will be discussing polarized lens. How they work, how they’re made, and why they are so, so useful for clarity and vision.
We hope you have enjoyed this long answer to a short question. Next time on Eye to the Future, we will be discussing polarized lens. How they work, how they’re made, and why they are so, so useful for clarity and vision.