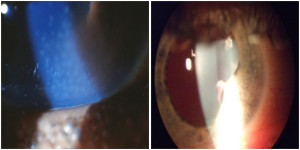
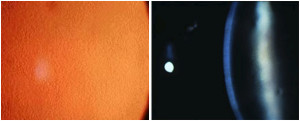
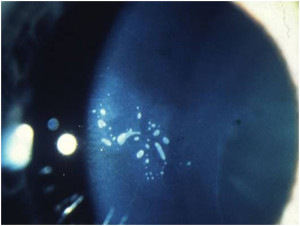
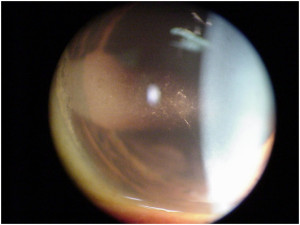
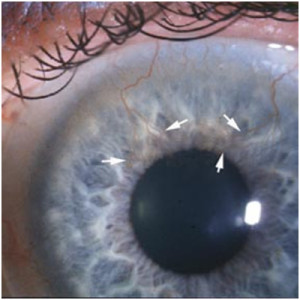
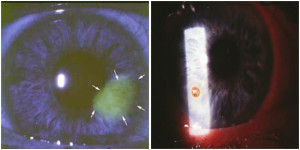
- Characterized by inflammatory cells and proteins in the anterior chamber of the eye
- Usually idiopathic
- Recurrent cases should be evaluated with lab tests for autoimmune diseases
Management
- Steroid regimen (dosing is severity dependent) with gradual taper to avoid rebound inflammation
- Cycloplegic agent to decrease inflammation, improve comfort, and prevent synechia of the iris